60 y/o male with hypertension, heart failure and decreased urine output
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Patient was apparently asymptomatic 3 months ago, then he developed b/l pedal edema, initially extending only up to the ankles, which gradually progressed up to both the thighs, over the last 15 days.
Patient c/o decreased urine output since 15 days
c/o SOB Grade 2 , No aggravating or relieving factors.
History of Past Illness
K/C/O HTN since 6 months
N/K/C/O DM, EPILEPSY, THYROID DISORDERS.
NO H/O CAD, ASTHMA, TB
NO H/O PRIOR HOSPITALISATIONS, surgeries or blood transfusions.
Personal History
Married
farmer by occupation
Appetite- Normal
Non Vegetarian
Bowel movements- regular
Occasionally drinks Alcohol
Smoker
No h/o drug use
Family History:
No Significant Family history
PHYSICAL EXAMINATION
General Examination:
Patient is C/C/C
Thin Build,
No pallor, icterus, cyanosis, edema, lymphadenopathy
VITALS:
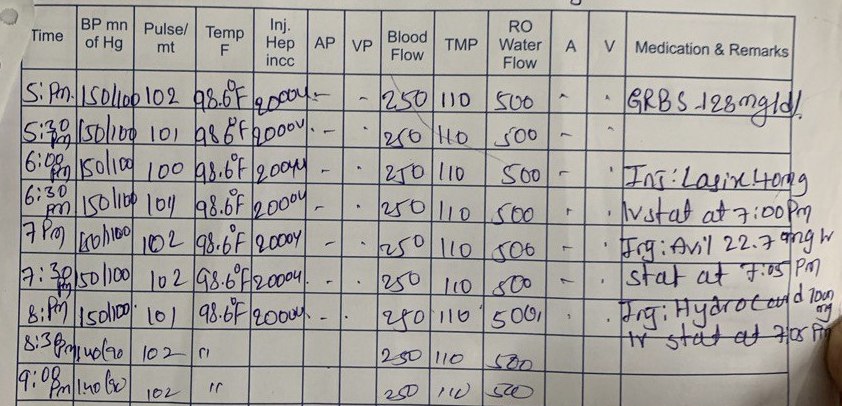
Temp: 100 F
PR:98 bpm
RR:29 cpm
BP:
Lt arm:150/80 mm Hg
Rt arm:140/80 mm Hg
SpO2 : 84 % RA
GRBS: 124 mg/dl
SYSTEMIC EXAMINATION:
GIT:
Shape- Scaphoid
All quadrants of the abdomen are moving accordingly to respiration.
No tenderness, guarding.
On palpation, abdomen is soft, no hepatosplenomegaly.
Hernial orifices are normal.
No bruits
Bowel sounds are heard
Genitals- Normal.
CNS EXAMINATION:
Mental Status:
Patient was conscious, coherent ,cooperative. Well oriented to time, place and person.
Language: Fluent, able to name relatives, follows commands
Cranial Nerves- intact
Motor:
Upper Limb:
Pronator drift absent.
Tone:
Increased in both Upper and Lower limbs, asymmetrically.
Power:
Upper Limbs:3/5 in both limbs
Lower limbs: 2/5 in both limbs
Tremors:
Fine tremor present when arms are outstretched.
Posture:
On standing, patient is seen to be stooping.
Patient unable to walk by himself, needs support to stand and walk.
Finger to Nose Testing:
Normal
Rapid alternating Movements : Normal
Romberg: Negative
Proprioception:
Reflexes: Not able to elicit.
Babinski: Flexor response
Sensory Examination
Vibration: Normal
Joint position sense : Normal
Pin prick, temperature sensation: Normal
CVS:
S1, S2 Heard, No murmurs
RS:
Dyspnoea: Present
BAE present, NVBS heard
No adventitious sounds
INVESTIGATION
Hemogram
1/12/23
Ecg
Electrolytes











Comments
Post a Comment